Introduction
One of the most essential systems in the human body, the respiratory system transports oxygen to cells and eliminates metabolic waste, carbon dioxide. Maintaining health and addressing respiratory disorders requires knowledge of the respiratory system’s anatomy, physiology, and pathology. This blog covers the respiratory system’s structure, function, and joint disorders.
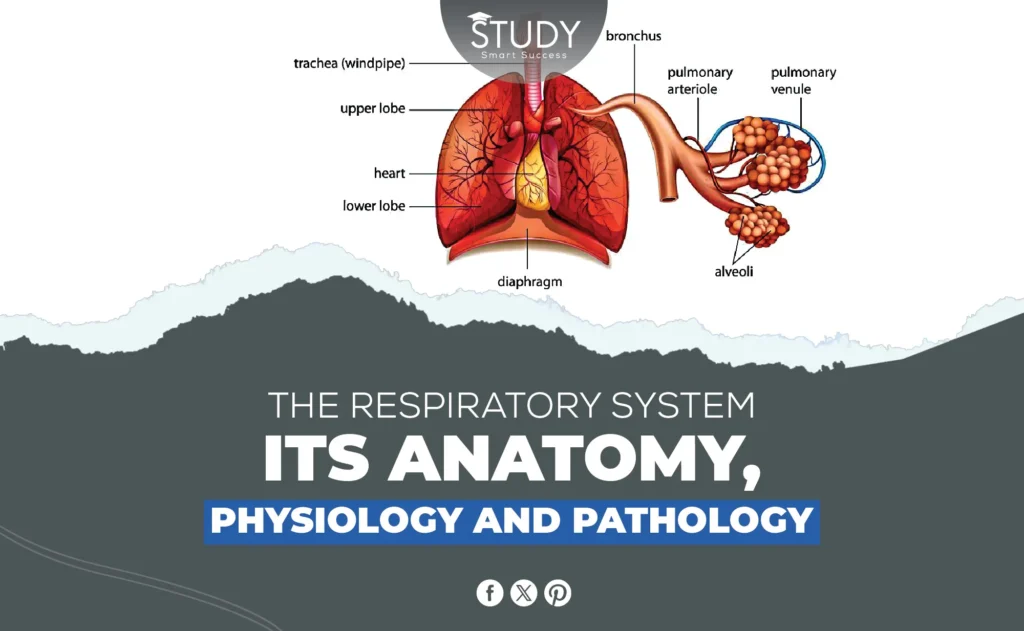
Anatomy of the Respiratory System
Major Structures
Nose and Nasal Cavity:
Air enters the respiratory system through the nose and nasal cavity. They are essential for filtering dust, germs, and other particles from the air. Humidifying and warming the air in the nasal cavity makes it better for the sensitive lower respiratory tract tissues.
Pharynx and Larynx:
The throat, or pharynx, is a muscular tube that transports air and food. Voice is produced by the larynx, positioned below the pharynx. The larynx protects the trachea from food and liquids while swallowing.
Trachea and Bronchi:
The stiff trachea connects the larynx to the bronchi. C-shaped cartilage rings support the trachea and prevent collapse during breathing. The trachea has two lung-specific main bronchi. These bronchi branch into bronchioles to deliver air throughout the lungs.
Lungs:
The respiratory system’s central organ, the lungs, exchange oxygen and carbon dioxide. Each lung has three right and two left lobes. Bronchioles branch into smaller passageways and form alveoli in each lobe. The tiny air sacs called alveoli exchange gas, making respiration possible.
Alveoli:
Alveoli are tiny balloon-like structures with enormous gas exchange surfaces. Each alveolus has capillaries that carry oxygen and carbon dioxide out of the blood. Adequate respiration requires alveoli to form and function to take oxygen and exhale carbon dioxide.
Diaphragm and Intercostal Muscles:
Breathing relies on the dome-shaped diaphragm beneath the lungs. Flattening the diaphragm creates a vacuum that sucks air into the lungs. The intercostal muscles between the ribs help breathe by extending and contracting the chest cavity. These muscles keep airflow smooth in and out of the lungs.
The Pleural Membrane
Function and Importance in Lung Protection:
Double-layered pleural membranes surround the lungs. It protects the lungs from chest wall friction during breathing. The pleural membrane maintains negative pressure for lung expansion.
Description of Pleural Cavity and Fluid:
The pleural cavity is the space between pleural membrane layers. The modest amount of pleural fluid in this space lubricates surfaces and helps the lungs breathe. Pleural fluid adheres to the lungs and chest wall, allowing inhalation expansion.
Physiology of the Respiratory System
The Process of Breathing
Inhalation:
Draw air into the lungs through inhalation. The dome-shaped diaphragm at the base of the lungs contracts first. When the diaphragm contracts, it flattens, expanding the thoracic cavity. The ribcage lifts, and the chest cavity expands when the intercostal muscles flex. Air flows through the nose or mouth, down the trachea, and into the lungs as the lungs expand and create negative pressure.
Exhalation:
Passive or active exhalation occurs. Passive exhalation relaxes the diaphragm and intercostals, shrinking the thoracic cavity. This volume reduction raises lung pressure, forcing air out. Active exhalation with speech or exercise requires more muscle. The abdominal and internal intercostal muscles contract, squeezing the chest cavity and expelling air more forcefully.
Gas Exchange Mechanism
Oxygen Transport:
In the lungs’ alveoli, oxygen is transported. When we breathe, oxygen-rich air fills our alveoli. Thin alveolar walls and capillaries allow oxygen to diffuse into the circulation. Red blood cell hemoglobin molecules deliver oxygen via the bloodstream to tissues and organs for cellular respiration.
Carbon Dioxide Removal:
Cellular respiration waste carbon dioxide is carried from tissues to the lungs for evacuation. It diffuses from cells into the bloodstream and reaches the lungs as bicarbonate ions. Carbon dioxide from the blood enters the alveoli and is exhaled during expiration.
Regulation of Breathing
Respiratory Centers in the Brain:
The brainstem’s medulla oblongata and pons respiratory centers control breathing. The medulla oblongata sends respiratory muscles to determine the basic breathing rhythm, whereas the pons adjust breathing rate and depth to physiological needs.
Chemoreceptors:
Chemoreceptors measure blood carbon dioxide, oxygen, and pH. Cor carotid arteries and aorta receptors alert the brain’s respiratory centers to imbalances like high carbon dioxide or low oxygen. To restore balance, the brain modulates breathing rate and depth.
Voluntary vs Involuntary Breathing:
Breathing is voluntary and involuntary. Without conscious effort, the brainstem controls involuntary breathing to maintain oxygen levels. However, voluntary breathing lets us control our respiratory patterns like speaking, singing, and holding our breath. The cerebral cortex can temporarily override the involuntary system to control voluntary behavior.
The Role of the Respiratory System in pH Balance
CO2 and Blood pH:
The respiratory system regulates carbon dioxide levels to maintain pH balance. Carbon dioxide dissolves in blood to generate carbonic acid, which dissociates into hydrogen and bicarbonate ions. The bicarbonate buffer system stabilizes blood pH via this procedure.
Hyperventilation and Hypoventilation:
Rapid breathing, or hyperventilation, lowers blood carbon dioxide levels, making it more alkaline. Respiratory acidosis occurs when carbon dioxide builds up in the blood due to hypoventilation, or slow, shallow breathing. The respiratory system constantly changes breathing to maintain blood pH equilibrium.
Pathology of the Respiratory System
Common Respiratory Disorders
Asthma:
Asthma is a chronic respiratory illness that causes airway inflammation and constriction, causing breathing difficulties. Family history, allergies, and respiratory infections all contribute to asthma. Common symptoms include wheezing, shortness of breath, chest tightness, and coughing, especially at night or early morning. Standard asthma treatment includes inhaled corticosteroids for inflammation reduction and bronchodilators for symptom relief.
Chronic Obstructive Pulmonary Disease (COPD):
COPD, a progressive condition, restricts lung airflow, making breathing difficult. It generally involves emphysema and chronic bronchitis. Chronic exposure to irritants like cigarette smoke, air pollution, and occupational toxins increases COPD risk. Symptoms include chronic cough, sputum, and breathlessness. Quality of life is improved by smoking cessation, bronchodilators, inhaled steroids, and pulmonary rehabilitation.
Pneumonia:
One or both lung air sacs are inflamed by pneumonia. Fluid or pus in the air sacs can cause coughing, phlegm, fever, chills, and difficulty breathing. Bacterial pneumonia is the most prevalent form. Antibiotics, antivirals, and antifungals may be used with supportive care to treat symptoms, depending on the etiology.
Tuberculosis:
TB is a dangerous infectious disease caused by Mycobacterium tuberculosis. The lungs are its primary target, but it can spread. A chronic cough, weight loss, nocturnal sweats, and fever are symptoms. Airborne droplets propagate extremely infectious TB. TB is still a global problem, especially in developing nations. Multiple antibiotics are prescribed for six months or longer.
Respiratory System and Infections
Viral Infections (e.g., Influenza, COVID-19):
Influenza and COVID-19 can severely damage the respiratory system. Fever, cough, shortness of breath, and exhaustion might result from airway and lung inflammation from these infections. They can cause pneumonia or ARDS in extreme situations. Supportive treatment relieves symptoms and prevents complications.
Bacterial Infections:
Bacteria can cause pneumonia, bronchitis, and tuberculosis, impairing lung function. Thick mucus, fever, and respiratory problems commonly accompany these diseases. Most bacterial infections are treated with antibiotics, and early management prevents consequences.
Fungal Infections:
Though rare, respiratory fungal infections can be severe, especially in immunocompromised people. Lung fungal infections include aspergillosis and histoplasmosis. Chronic cough, chest pain, and breathing problems are symptoms. Treatment usually involves antifungals.
Cancer of the Respiratory System
Lung Cancer:
Lung cancer is one of the most frequent and deadly cancers caused by smoking, radon gas, asbestos, and other environmental causes. There are two main types: SCLC and NSCLC. A prolonged cough, chest pain, hoarseness, weight loss, and bloody cough are symptoms. Surgery, chemotherapy, radiation therapy, and targeted medication therapies may be used depending on the cancer kind and stage.
Prevention and Early Detection:
Smoking and hazardous drugs are risk factors for lung cancer. At-risk populations need regular screenings like low-dose CT scans for heavy smokers to improve survival chances. Early diagnosis also requires awareness and education about lung cancer symptoms.
Respiratory Failure
Acute Respiratory Distress Syndrome (ARDS):
Fluid buildup in the alveoli causes severe shortness of breath and hypoxia, causing ARDS. Severe infections, trauma, and inhalation injuries can cause it. ARDS requires rapid medical intervention, including mechanical ventilation and supportive care, to treat underlying causes.
Chronic Respiratory Failure:
COPD or severe chronic asthma causes gradual persistent respiratory failure. It occurs when the respiratory system cannot sustain blood oxygen and carbon dioxide levels. Long-term oxygen therapy, lung function medicines, and non-invasive ventilation may help breathe. The goal is to improve quality of life and manage symptoms.
Preventive Measures and Healthy Habits
Lifestyle Changes to Support Respiratory Health
Avoiding Smoking and Secondhand Smoke:
The primary cause of respiratory disorders, including COPD and lung cancer, is smoking. The chemicals in tobacco smoke damage the airways and alveoli, reducing lung function and increasing respiratory infections. Passive smoking is very hazardous, especially for children and non-smokers. One of the best strategies to safeguard lung health is to avoid smoking and secondhand smoke.
Exercise and Fitness:
Regular exercise improves lung function. Exercise boosts lung capacity, respiratory muscle strength, and oxygen exchange efficiency. Aerobic workouts, including walking, jogging, and swimming, improve respiratory health. Staying active helps manage weight, reduce respiratory strain, and boost cardiovascular health.
Environmental Factors
Pollution and Air Quality:
Air pollution is a significant respiratory health risk. Particulate particles, ozone, and nitrogen dioxide can inflame airways, worsen asthma, and increase respiratory infections. Monitor air quality, especially in urban areas, and limit outside activities on high pollution days or use air purifiers indoors to reduce exposure.
Occupational Hazards:
Dust, chemicals, and fumes in several jobs might harm respiratory health. Construction, mining, and manufacturing workers are more likely to get asbestosis, silicosis, and occupational asthma. Wearing protective gear, following safety rules, and ensuring workplace ventilation reduces exposure to dangerous compounds.
Nutrition and Respiratory Health
Dietary Choices:
Balanced diets with fruits, vegetables, whole grains, and lean proteins improve lung health. Antioxidant-rich foods like vitamins C and E decrease inflammation and protect lung tissue. Omega-3 fatty acids in salmon and flaxseeds reduce inflammation and assist asthmatics and other respiratory patients. Eat healthy to avoid obesity, which can compromise lung function.
Supplements:
Respiratory health depends on vitamins and minerals. Asthmatics can enhance lung function and prevent respiratory infections with vitamin D. Magnesium relaxes respiratory muscles, improving airflow. Before taking supplements, visit a doctor because everyone’s needs differ.
Vaccinations and Regular Health Check-ups
Importance of Vaccinations:
Respiratory infections are prevented with vaccinations. The influenza and pneumococcal vaccines protect against common respiratory viruses that can cause serious illness in vulnerable individuals like the elderly and those with chronic health conditions. Vaccinations are essential to preventing respiratory infections.
Screening for Respiratory Disorders:
Early detection and treatment of respiratory problems require regular health checkups. When asthma, COPD, and lung cancer are early and treatable, lung function tests, chest X-rays, and other diagnostic methods can detect them. Early intervention can stop these diseases and enhance respiratory patients’ lives.
Conclusion
Respiratory health includes good lifestyle choices, environmental awareness, correct nutrition, and frequent medical care for complete well-being. Avoiding smoking, being active, eating a balanced diet, and getting immunizations and checkups help lower the incidence of respiratory illnesses and improve lung function. Understand and follow these preventive actions to build a healthier, more resilient respiratory system, making breathing more accessible and fulfilling.